Imagine this scenario: You’re going about your day, and unexpectedly, you experience a sudden jolt or impact to your spine. Ouch! It’s painful, and you might be wondering what just happened and what it means for your health. In this article, we will explore how spinal trauma can increase the likelihood of disc protrusion, shedding light on the connection between these two discomforting experiences. So, sit back, relax, and let’s dive into the fascinating world of spinal health together.
Overview of Spinal Trauma
Spinal trauma refers to any injury or damage to the spinal cord or surrounding structures, such as the vertebrae, discs, and ligaments. It can result from various causes, including accidents, falls, sports injuries, and violence. Spinal trauma can have serious consequences on a person’s overall health and quality of life, as it can lead to neurological deficits, chronic pain, and functional limitations.
Definition of spinal trauma
Spinal trauma is defined as any injury or trauma to the spinal cord, vertebrae, or surrounding structures. It can range from minor fractures to severe injuries that result in spinal cord compression or damage.
Types of spinal trauma
Spinal trauma can be categorized into different types based on the severity and location of the injury. These include:
- Spinal fractures: The vertebral bones can fracture due to trauma, leading to instability and potential damage to the spinal cord.
- Spinal cord injuries (SCI): These occur when the spinal cord is compressed, bruised, or severed, resulting in varying degrees of sensory, motor, and autonomic function loss.
- Spinal ligament injuries: The ligaments that stabilize the spine can be sprained or torn, causing instability and pain.
- Disc herniation: Trauma can cause a disc to protrude or herniate, which can lead to nerve compression and pain.
Causes of spinal trauma
Spinal trauma can result from various causes, including:
- Motor vehicle accidents: Collisions, impacts, or sudden decelerations can cause significant spinal trauma.
- Falls: Accidental falls from heights or slips and trips can result in spinal injuries, particularly among older adults.
- Sports injuries: High-impact sports, contact sports, and activities with a risk of trauma, such as diving or gymnastics, can lead to spinal injuries.
- Violence: Physical assault, gunshots, or other forms of intentional trauma can cause severe spinal damage.
- Work-related accidents: Certain occupations, such as construction or heavy-lifting jobs, can increase the risk of spinal trauma.
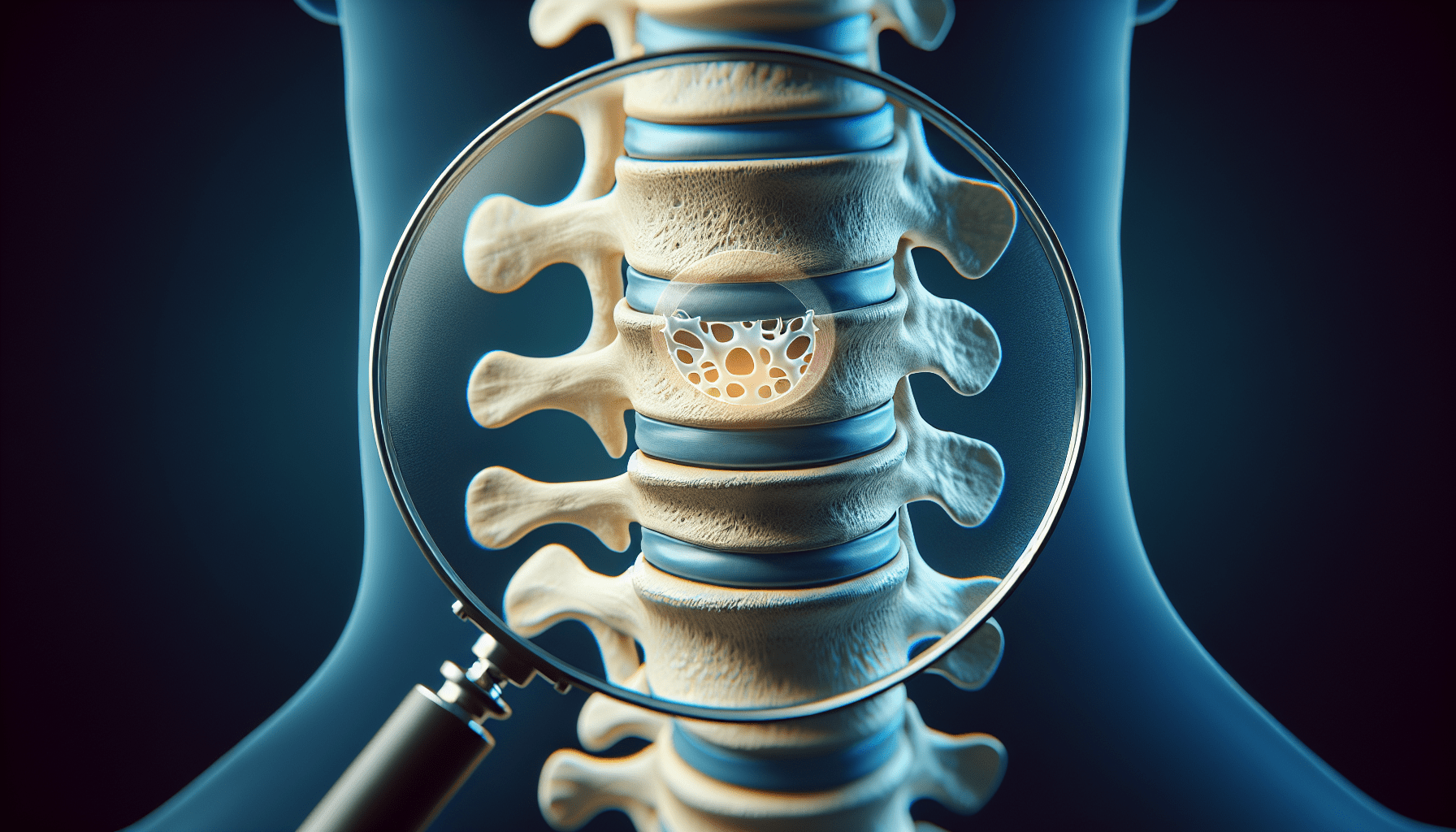
Understanding Disc Protrusion
Disc protrusion is a common spinal condition that can occur as a result of spinal trauma, among other causes. It involves a bulging or protrusion of the intervertebral disc, which serves as a cushion between the vertebrae. When a disc protrudes, it can exert pressure on nearby nerves, causing pain and other symptoms.
Definition of disc protrusion
Disc protrusion refers to the abnormal bulging or protrusion of the intervertebral disc, which can compress nearby nerve roots or the spinal cord itself. It is often accompanied by degenerative changes in the disc structure.
Common symptoms of disc protrusion
Disc protrusion can cause a range of symptoms, including:
- Back pain: Pain in the affected area of the spine, which may radiate to the buttocks, legs, or arms.
- Numbness or tingling: Sensations of numbness, tingling, or a “pins and needles” feeling in the extremities.
- Muscle weakness: Weakness or difficulty in performing certain movements or activities.
- Changes in sensation: Altered feeling, such as a loss of sensation or heightened sensitivity in specific areas of the body.
- Loss of bladder or bowel control: Severe cases of disc protrusion can compress the spinal cord, leading to a loss of control over bladder and bowel function.
Causes of disc protrusion
While spinal trauma can increase the likelihood of disc protrusion, it is not the sole cause of this condition. Other contributing factors may include:
- Degenerative changes: Age-related wear and tear on the intervertebral discs can weaken their structure and make them more prone to protrusion.
- Repetitive stress: Activities or occupations that involve repetitive motions or heavy lifting can increase the risk of disc protrusion.
- Poor posture and body mechanics: Maintaining prolonged poor posture or using incorrect body mechanics can place excessive stress on the spine, potentially leading to disc protrusion.
- Sedentary lifestyle: Lack of regular exercise and physical activity weakens the supporting structures of the spine, making disc protrusion more likely.
- Genetic factors: Some individuals may have a genetic predisposition to developing disc protrusion or other spinal conditions.
Connection between Spinal Trauma and Disc Protrusion
Spinal trauma can have a direct impact on the spinal structures, increasing the likelihood of disc protrusion. The mechanism of disc protrusion itself involves changes in the intervertebral discs due to trauma, leading to their protrusion or herniation.
Impact of spinal trauma on the spine
Spinal trauma can cause fractures, dislocations, or other injuries to the vertebrae, resulting in instability and misalignment of the spine. This instability can lead to abnormal forces being exerted on the intervertebral discs, making them more susceptible to damage or protrusion.
Mechanism of disc protrusion
Following spinal trauma, the intervertebral discs can experience structural changes, such as tears or weakening of the outer annulus fibrosus. This can allow the gel-like inner nucleus pulposus to bulge or herniate outwards, pressing against nearby nerves or the spinal cord.
Risk factors for disc protrusion after spinal trauma
Several factors can increase the likelihood of disc protrusion following spinal trauma, including:
- Severity of trauma: The extent and severity of spinal trauma can influence the likelihood of subsequent disc protrusion.
- Location of trauma: Injuries to specific areas of the spine, such as the lumbar region, may have a higher association with disc protrusion.
- Age: Older individuals may be at a higher risk of disc protrusion due to the degenerative changes that occur naturally in the intervertebral discs over time.
- Inadequate rehabilitation: Insufficient or inadequate rehabilitation following spinal trauma can contribute to reduced spinal support, leading to disc protrusion.
Effects of Spinal Trauma on Intervertebral Discs
Spinal trauma can have profound effects on the structure and function of the intervertebral discs. These effects can result in a disruption of disc integrity, inflammation, and degeneration.
Changes in disc structure and function
Spinal trauma can cause tears or fissures in the outer annulus fibrosus of the intervertebral disc, which compromises its ability to withstand and distribute forces. This can lead to decreased disc height and altered load-bearing capacity.
Disruption of disc integrity
Trauma can disrupt the normal structure and alignment of the intervertebral discs, which can result in instability and abnormal motion within the spinal segments. This disruption can contribute to disc degeneration and increase the risk of disc protrusion.
Inflammation and degeneration of discs
Spinal trauma can trigger an inflammatory response in the intervertebral discs, leading to the release of inflammatory mediators and pro-inflammatory cytokines. This chronic inflammation can contribute to disc degeneration over time, further increasing the likelihood of disc protrusion.
Biomechanical Factors in Spinal Trauma-related Disc Protrusion
Several biomechanical factors play a role in the development of disc protrusion following spinal trauma. These factors can contribute to increased stress on the intervertebral discs and compromise their structural integrity.
Increased axial load on discs
Spinal trauma can cause an increase in axial load, or the force exerted along the spine, which can place additional stress on the intervertebral discs. This increased load can contribute to the weakening and degeneration of the discs, increasing the risk of disc protrusion.
Loss of disc height and hydration
Following trauma, the intervertebral discs may lose their normal height and hydration, making them more susceptible to damage. Disc dehydration can result in reduced shock absorption and load distribution, further increasing the likelihood of disc protrusion.
Altered disc mechanics and distribution of forces
Trauma can disrupt the normal mechanics and distribution of forces within the intervertebral discs. This can lead to abnormal loading patterns and uneven stress distribution, increasing the risk of disc protrusion in certain areas of the spine.
Role of Inflammatory Response in Disc Protrusion
Inflammation plays a significant role in the development and progression of disc protrusion following spinal trauma. The inflammatory response triggered by trauma can contribute to disc degeneration and increase the likelihood of disc protrusion.
Inflammatory mediators and cytokines
Following spinal trauma, the intervertebral discs can release inflammatory mediators and pro-inflammatory cytokines, such as interleukin-1 and tumor necrosis factor-alpha. These substances can contribute to disc degeneration and the development of disc protrusion.
Immune cell infiltration in injured discs
In response to trauma and inflammation, immune cells can infiltrate the injured intervertebral discs. These immune cells release additional inflammatory substances and enzymes that further contribute to disc degeneration and the risk of disc protrusion.
Potential mechanisms linking inflammation to disc protrusion
The exact mechanisms linking inflammation to disc protrusion following spinal trauma are not fully understood. However, it is believed that the inflammatory process can compromise the structural integrity of the intervertebral discs, leading to weakened areas that are more likely to herniate or protrude.
Diagnostic Methods for Spinal Trauma and Disc Protrusion
Various diagnostic methods are available to assess spinal trauma and identify disc protrusion. These methods can help healthcare professionals accurately diagnose the condition and determine appropriate treatment options.
Imaging techniques (X-ray, MRI, CT scan)
Imaging techniques such as X-ray, magnetic resonance imaging (MRI), and computed tomography (CT) scan can provide detailed images of the spinal structures. These imaging modalities allow for the visualization of fractures, disc protrusion, and other abnormalities associated with spinal trauma.
Physical examination and clinical assessments
The healthcare provider may perform a physical examination and various clinical assessments to evaluate the patient’s symptoms, range of motion, neurological function, and other relevant factors. This can help determine the presence and extent of spinal trauma and associated disc protrusion.
Discography and discogram
Discography and discogram are specialized diagnostic procedures that involve the injection of a contrast dye into the intervertebral discs. These procedures can help identify the specific disc(s) causing the symptoms and assess their structural integrity.
Treatment Options for Spinal Trauma and Disc Protrusion
The treatment approach for spinal trauma and associated disc protrusion depends on the severity of the condition, the presence of neurological deficits, and the patient’s overall health. Treatment options can vary from conservative approaches to surgical interventions.
Conservative approaches (rest, physical therapy)
Conservative treatment options for spinal trauma and disc protrusion may include:
- Rest and activity modification: Giving the spine time to heal and avoiding activities that exacerbate symptoms.
- Physical therapy: Specialized exercises and techniques to improve strength, flexibility, and posture, as well as alleviate pain and support proper spinal alignment.
- Pain management techniques: Utilizing modalities such as heat or cold therapy, transcutaneous electrical nerve stimulation (TENS), and nonsteroidal anti-inflammatory drugs (NSAIDs) to manage pain and inflammation.
Medications (NSAIDs, pain relievers)
Medications can be prescribed to manage pain and inflammation associated with spinal trauma and disc protrusion. Nonsteroidal anti-inflammatory drugs (NSAIDs), analgesics, muscle relaxants, and corticosteroids are commonly used to provide relief and improve symptoms.
Surgical interventions (disc herniation removal, fusion)
In severe cases of spinal trauma and disc protrusion, surgical intervention may be necessary. Surgical procedures may involve removing the herniated or protruding disc material (discectomy) or stabilizing the spine through spinal fusion. These surgeries aim to alleviate symptoms, restore spinal stability, and improve overall function.
Prevention and Rehabilitation Strategies
Prevention and rehabilitation strategies play a crucial role in minimizing the risk of spinal trauma and supporting recovery following an injury.
Proper ergonomics and body mechanics
Maintaining proper ergonomics and body mechanics can help reduce the risk of spinal trauma and associated disc protrusion. This involves maintaining good posture, lifting heavy objects correctly, and using ergonomic equipment or modifications in work and daily activities.
Strengthening exercises for spinal support
Engaging in regular exercises that strengthen the muscles supporting the spine can help prevent spinal trauma and reduce the likelihood of disc protrusion. Core strengthening exercises, targeted back exercises, and exercises that improve posture and flexibility can provide significant benefits.
Post-injury rehabilitation programs
Following spinal trauma and disc protrusion, rehabilitation programs can help restore function, improve mobility, and reduce the risk of recurrent injuries. These programs often involve a combination of physical therapy techniques, exercises, and education on proper body mechanics and injury prevention strategies.
Prognosis and Long-Term Outlook
The prognosis and long-term outlook for individuals with spinal trauma and disc protrusion can vary depending on several factors, including the severity of the injury, the effectiveness of treatment, and individual factors such as age and overall health.
Recovery rates and timeframes
Recovery rates and timeframes following spinal trauma and disc protrusion can vary widely. Mild cases may resolve within a few weeks to months with conservative treatment, while more severe cases may require longer recovery periods and ongoing rehabilitation.
Potential complications and recurrence
Complications from spinal trauma and associated disc protrusion can include chronic pain, neurological deficits, and decreased quality of life. Additionally, there is a risk of recurrence or the development of new disc protrusions in the same or adjacent spinal segments over time.
Importance of ongoing care and monitoring
Due to the potential for complications and recurrent disc protrusion, ongoing care and monitoring are essential for individuals with spinal trauma. Regular follow-up appointments and adherence to recommended treatments and rehabilitation programs can help manage symptoms, prevent further damage, and optimize long-term outcomes.
In conclusion, spinal trauma increases the likelihood of disc protrusion due to the impact on the spine, disruption of disc integrity, biomechanical factors, inflammatory response, and other complex mechanisms. Understanding the connection between spinal trauma and disc protrusion can aid in diagnosis, treatment, and prevention strategies, ultimately improving the prognosis and long-term outlook for individuals affected by these conditions.
